FAQ
Why are insurance companies doing this?
Money. Specialty drugs for patients with cancer, AIDS, and other life-threatening diseases are very expensive—sometimes running in the tens of thousands of dollars per prescription—and big insurance companies are trying to increase their profits on these expensive drugs. It’s sold as a cost-saving measure, but there is no guarantee that any savings will be passed to consumers or employers.
How would they do this?
It’s fairly complicated, but essentially insurance companies set the drug price through companies they now own (pharmacy benefit managers) and then pay themselves whatever price they set.
What’s a pharmacy benefit manager?
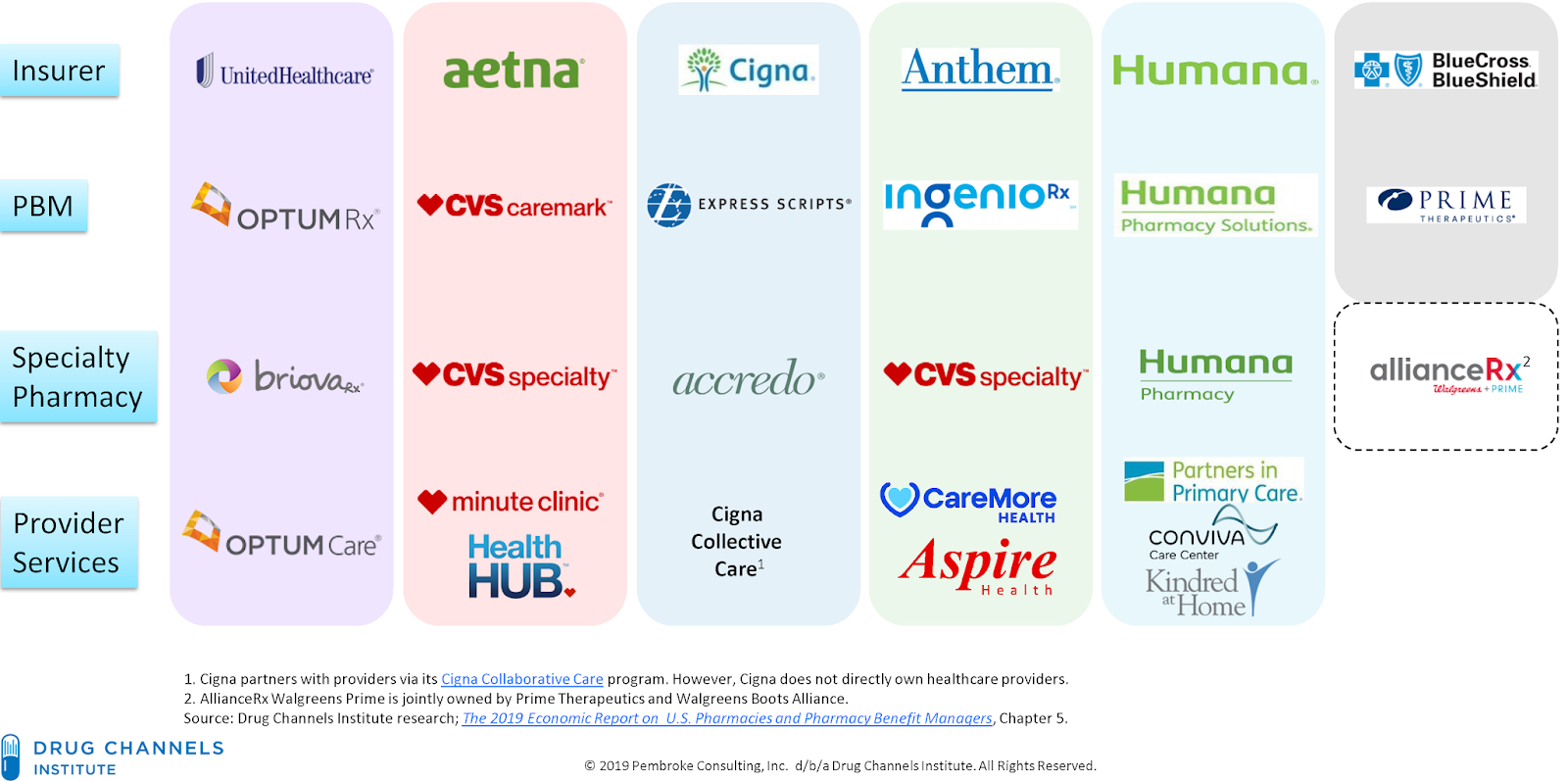
Started in the 1960s, pharmacy benefit managers, or PBMs, were designed to process the substantial number of “small-dollar” prescription drug claims for insurance companies and plan sponsors. They used their large purchasing power to negotiate prices with pharmaceutical manufacturers and impact almost every aspect of the prescription drug marketplace.
As coverage expanded with the inception of the Medicare Part D program in 2006 and the Affordable Care Act in 2010, insurance companies became more interested in PBMs since they have a significant behind-the-scenes impact in determining total drug costs for insurers, shaping patients’ access to medications, and determining how much pharmacies are paid.
Today, the 5 largest insurance companies now own their own PBMs:
Why is this bad for Hoosiers?
With drug prices continuing to rise, state lawmakers, businesses, and other entities that serve Hoosiers are questioning if big insurance companies are abusing their power through their integrated PBMs and specialty pharmacies and pocketing large savings from pharmaceutical manufacturer rebates that, in theory, should be passed down to consumers.
Insurance companies own the PBMs and the PBMs own the specialty pharmacies, so they are setting their own price and paying themselves, making exorbitant profits and charging their members – Hoosier businesses and consumers – via higher premiums.
How do insurance companies know what the patient needs?
They don’t. Hoosiers undergoing infusion therapy are often evaluated on the same day as their scheduled treatment. Depending on lab results, imaging, and clinical presentation, initial treatment plans may be amended or cancelled altogether. The specialty drugs brought/sent to the infusion center may no longer be the appropriate regimen. At a minimum, this means causing inconvenience and patient dissatisfaction because of a rescheduled appointment and possibly wasting expensive drugs. But the implications are much greater — this likely means a delay in treatment that increases the risk of adverse outcomes and hampers recovery.
How safe are “white bagged” drugs?
With mandatory white bagging, providers don’t know how these drugs were stored or prepared before they are delivered to the facility administering the drugs. Patient safety is a critical concern. When a drug is delivered to a facility/office through this process, the health care provider responsible for infusing that therapy is now forced to address questions such as: Was it properly refrigerated? How and when was it mixed or compounded? Specialty drugs are complex and require special attention to ensure accuracy and safe handling.
How greatly will these policies reduce access?
Many providers will be unwilling to expose their patients to what they believe is unreasonable clinical risk and will not infuse white bagged drugs. This could significantly impair access to medically appropriate care and result in patents having to travel significant distances for their infusions.
Why do hospitals mark up the price of drugs?
Hospitals mark up the price of drugs to cover the costs of storing, handling, clinically reviewing the patient’s treatment plan and drug order, compounding the drug in a safe, sterile environment, and checking the compounded product for safety and accuracy – all done by licensed, trained health care professionals. All of this work requires expensive equipment and engineering controls, supplies, and labor. In addition, a hospital must cover unreimbursed costs of patient care and insurance administration.
While it is correct that hospitals mark up the price of drugs, this is something that can be easily addressed and negotiated within the hospital contracting process. On the other hand, PBMs that are owned by insurance companies, own their own pharmacies and frequently markup drugs to a much greater extent and with no transparency to the public because, for these transactions, the insurers are “paying themselves” for these drugs and they do not appear on provider claims. Instead, it is an “off the record” transaction.
Why is Hoosiers for Safe Meds asking the legislature to intervene in private contract negotiations?
Hoosiers for Safe Meds is not asking the legislature to intervene in private contract negotiations. Physicians, hospitals, and insurance companies should privately negotiate their contracts. What shouldn’t be allowed is the threat of an unsafe alternative in this process. Insurance companies can choose to renegotiate their contracts and rates at any time. The State should protect their residents against these unsafe practices mandated by insurers.
Make your voice heard today.
Has your care been delayed due to mandatory white bagging? Share your story with us. Contact your elected officials and make your voice heard as the State considers the safety implications of these practices. Together we can create real change.